Jot down the first thing that comes to your mind.
Tag: USA
-
Big thoughts.. inspired this long winded blog 😂
-
Addressing the Paramedic Shortage Crisis in America

“Critical Condition: The Paramedic Shortage in America”
A System in Crisis
A system in crisis? You might be surprised to learn how few paramedics are working in your town right now. What about in Mississippi? Or the entire United States? Shockingly, the numbers reveal a massive shortage—and it’s getting worse.
But emergencies don’t stop happening just because we don’t have enough paramedics.
Imagine this: someone you love is having a heart attack. You call 911, panicked, desperate for help. But what if no paramedic is available to respond? What would you do?
Sure, you could pray. You could throw them in the car and speed to the nearest hospital. But what if time’s not on your side? What if they go downhill while you’re driving?
Scary thought, right? Unfortunately, this is the reality in many places across the country.
As of 2025, the National Registry of Emergency Medical Technicians (NREMT) reports the following numbers of nationally certified EMS professionals in the United States:
- Emergency Medical Technicians (EMTs): 328,582 (65.1%)
- Advanced EMTs (AEMTs): 25,738 (5.1%)
- Paramedics: 134,208 (26.6%)
These figures sum to a total of 504,641 nationally certified EMS clinicians across the country.
Notice this is Across the country,
As of 2025, Mississippi has 1,938 licensed Emergency Medical Technicians (EMTs) and 1,765 licensed paramedics, according to the state’s emergency medical service information system. This totals 3,703 licensed EMS professionals statewide. Given Mississippi’s population of approximately 2.9 million, this equates to roughly 1 EMS provider per 783 residents.
I wish I could tell you we have enough first responders to handle the demand—but we don’t. Not only are we facing a shortage of paramedics, but EMTs and advanced EMTs too. And while those roles are critical to the EMS system, even with everyone working together, we’re still falling short.
This matters—to all of us.

In this blog, I’m going to take you behind the scenes of the EMS system. I’ll explain the structure, the responsibilities, and the strain we’re under. I’ll explore the numbers, the people, and the growing cracks in emergency medical services. But more importantly, I’ll answer the questions no one is asking: What do we really do? Why is the shortage happening? And how can you help?
The Heart of the Profession
A Day in the Life of a Paramedic
Typically, I set my alarm for around 4:30 a.m. I live about thirteen minutes from my station, so it gives me enough time to get into the right headspace before my shift. I get up, shower—unless I took one the night before—make my coffee, brush my teeth and hair, and start dressing for the day.
My uniform is practical, not just for professionalism but for protection. Tactical boots—because you never know when you’ll be stepping through shattered glass at a wreck scene or navigating through a neglected home. Tactical pants with a sturdy belt, uniform shirt, and my work bag packed with my stethoscope and other tools I might need. Before I leave, I say a quick prayer—because I never know if I’ll make it back home.
When I walk out that door, I’m aware of the risks. We face violent situations every day—drug abuse, uncooperative bystanders, reckless drivers who don’t yield even when we’re running lights and sirens. We’re at risk of being hit on the way to help someone else. We walk into scenes that no movie could prepare you for. Smells that burn your eyes. Frantic, high-emotion environments. Gunshot victims, overdoses, crashes, and just outright chaos.
Sure, law enforcement is supposed to have our backs—but sometimes we don’t realize we need them until it’s too late.
On my way to work, I try to mentally prepare for what the day might bring. When I get to the station, we check the truck—lights, sirens, and every piece of life-saving equipment. If we’re lucky, we get that done before the calls start. But some mornings, the tone drops before we’ve barely clocked in.
Early morning calls are usually never good. People wake up sick. People wake up to find a loved one has passed. And sometimes, it’s a crash on the way to work. Once the calls begin, we’re off—treating, transporting, cleaning the truck, and preparing for the next call. It doesn’t stop.
Calls range from routine transfers to the gut-wrenching scenes—deceased patients, abuse, trauma. We respond. We carry on. Because that’s what we do.
The Emotional and Physical Toll
We’re human. We feel things. We hurt. We care. And yes, sometimes we get frustrated—but we keep showing up.
There are times a person might call 911 three times in one day, and I wonder why they didn’t just call their doctor. But then I remind myself: It may not be an emergency to me, but it’s an emergency to them. That matters. So I treat them with the same respect as someone who’s coding. Sometimes all they need is a ride, or maybe they’re just lonely and need someone to talk to.
Then there are those moments—the ones that leave a mark. Walking into a stranger’s home with all eyes on you, expecting you to fix everything. To save someone who’s slipping away. Sometimes you can’t. And that’s the part that’s hardest. You have to keep your emotions tucked away, even when inside you’re falling apart.
But I’ve learned how to let go—at least the things I can’t control. If I gave it everything I had, I can walk away knowing I did my best.
And I’m an advocate. A voice. A protector. If I walk into a home and find someone—adult or child—who needs someone to stand up for them, I’m that someone. I may have been a stranger when I walked in, but I’ll fight for them like a mother bear for her cub.
Physically, the job has taken a toll. My back, knees, and hips have paid the price. Climbing in and out of a high ambulance has worn down my knees—I’m pretty sure I don’t have much cartilage left. The stretcher alone weighs 130 pounds, not counting the patient. I’ve gotten strong, but it’s a strength that’s come with pain.
Many of our medics who’ve been in the field for over ten years have had at least one surgery—knees, hips, shoulders—or they will after they retire. This job will wear you down. But we keep going. Because people need us.
Causes of the Shortage
Low Pay and Limited Career Advancement
Let’s be real—this profession doesn’t pay what it’s worth. Many of my coworkers work multiple EMS jobs and have side gigs outside of EMS just to make ends meet. Some are pulling long shifts at one job and heading straight to another. You could almost go flip burgers or take a job at a factory and make the same—if not more—than a trained EMT or paramedic with years of experience.
If you think your 9-to-5 is exhausting, try pulling a 48-hour shift with no guarantee of sleep, real food, or even time to sit down. Sure, we might get to shower or catch a nap between calls—if we’re lucky. But many times, it’s back-to-back emergencies. And these aren’t minor issues—we’re talking about trauma, death, abuse, addiction, violence.
One of my coworkers just finished his shift with nearly 200 hours on a two-week paycheck. Why? To catch up on bills. So his wife can stay home with their kids. This isn’t just a job to us—it’s survival. And for some, it’s the only way they know how to serve their families and their communities at the same time.
The minimum we work is a 12-hour shift. That’s the starting point. But for most, it’s far beyond that.
Burnout and Mental Health Challenges
These long hours don’t just wear us down physically—they eat at us emotionally and mentally. The human brain isn’t wired to process the amount of trauma we’re exposed to on a daily basis. You’re expected to roll up on the worst day of someone’s life, do what needs to be done, and then carry on to the next call like it didn’t just happen. Try getting a decent night’s sleep after watching a young child die. Or handling a domestic scene so violent you’re still shaking while trying to write the report.
Imagine sitting down for a quick bite, only to be called away after two bites of your meal. You rush off to another call, use half the equipment on the truck, and then come back to cold, soggy food in a Styrofoam container. French fries after a cardiac arrest scene? Yeah, not great. Especially when you’re wearing someone else’s blood or bodily fluids, and there’s no time to change yet.
Gas station food becomes a sad norm and eating too fast or too little starts messing with your stomach. It’s not healthy—but there’s rarely time to care.
Photo by Nataliya Vaitkevich on Pexels.com COVID-19’s Lasting Impact
The pandemic broke a lot of people. COVID-19 didn’t just stretch EMS thin—it pushed many of us past our limits. Some medics never came back. They left the field altogether. Others who stuck it out are still dealing with the aftermath—mentally, emotionally, and financially. We lost some of the best providers because the system failed to support them when they needed it most.
Retirement of Seasoned Medics
On top of that, we’re watching our seasoned medics retire in large numbers. These are the folks with the experience, the instinct, the training. You can’t replace that overnight. And the new hires? Many don’t last. They come in wide-eyed and eager, but once they experience that one traumatic call that shakes them to their core—they’re gone. We try to train them. We try to prepare them. But some things, you just have to live through to understand.
Certification and Training Barriers
Staying certified isn’t just time-consuming—it’s expensive. We’re required to have 48+ hours of continuing education every two years. Add to that:
- State certification renewals
- CPR, ACLS, PALS, and more
- Courses that cost money and time
- A system that often doesn’t reimburse or support those efforts
It is a lot for people who are already overworked and underpaid. The requirements are necessary, no doubt—but they become a barrier when there’s no system in place to make them more accessible or affordable.
The Domino Effect

Photo by Cu00e9sar Gaviria on Pexels.com Strain on Emergency Departments and Hospitals
The shortage of paramedics doesn’t stop at the ambulance bay doors—it rolls right into the emergency department, and from there, affects every part of the healthcare system.
Some people call an ambulance thinking it’ll get them into a hospital room faster. But that’s a myth. Even if you arrive in an ambulance, you still have to go through triage just like everyone else. And if the emergency room is full—which it often is—we’re stuck with that patient until a room opens up. Sometimes that’s 15 minutes. Other times, it’s over an hour. In some cases, if the patient is stable, we end up placing them in the lobby because there’s just nowhere else to go.
Now imagine an ER doctor has a patient who needs a higher level of care—maybe stroke care, trauma, or a burn unit. But guess what? If all the ambulances are tied up with other patients—whether those calls were truly emergencies or not—there’s no one available to make the transport. That patient sits and waits, and their outcome could suffer because of it.
Then there’s psychiatric patients—people who are a risk to themselves or others. They have to be monitored one-on-one in the ER. They need to be transported to a behavioral health facility, but only certain facilities will take them. And those facilities are sometimes hours away. If there’s no transport available, they stay boarded in the ER—sometimes for 24 hours or more—waiting for a ride or a bed. The entire flow of care is bottlenecked because of the EMS shortage.
It’s a chain reaction. And every link in that chain feels the pressure.
Longer Response Times
One of the most dangerous consequences of this shortage is longer response times. If all units are on calls—especially in areas with limited staffing—you could be waiting 30 minutes or more for an ambulance. And in an emergency, minutes matter.
Sometimes, the next available unit is 30+ miles away. And depending on the terrain, traffic, or weather, it can take even longer.
This delay could mean life or death.
Public Safety Risks
When emergency resources aren’t available, the entire community is at risk.
What happens if you call 911 and no ambulance is available? Do you wait? Do you drive yourself? What if you’re the one unable to breathe? What if it’s your child choking? Or your spouse having a stroke?
This isn’t a “maybe” scenario. It’s happening now.
The public often doesn’t realize how thin we’re stretched—until they need us and we aren’t there fast enough.
Impact on Rural vs. Urban Areas
This shortage affects everyone—but rural areas suffer the most.
In rural communities, EMS coverage is often limited to one or two trucks. If those are out on calls, there’s nothing left. Add in the long distances—winding backroads, hard-to-locate homes with no clear address markers—and it takes even longer to reach the scene.
Even finding the house can be a challenge if the mailbox is missing or house numbers aren’t visible. In some places, we have to drive until we spot someone flagging us down. That’s valuable time we can’t afford to waste.
Meanwhile, urban areas may have more resources, but they also have a higher volume of calls, denser traffic, and overcrowded ERs—so they’re not immune to delays either. The shortage of paramedics is not just an EMS problem. It’s a systemic problem—one that affects hospitals, doctors, patients, families, and entire communities.
This domino effect shows just how fragile the chain of emergency care really is.
The Human Side of the Shortage
Family Perspectives
My kids were 4,3,and 1 when I became a Paramedic. They are 18,17, and 14 now..
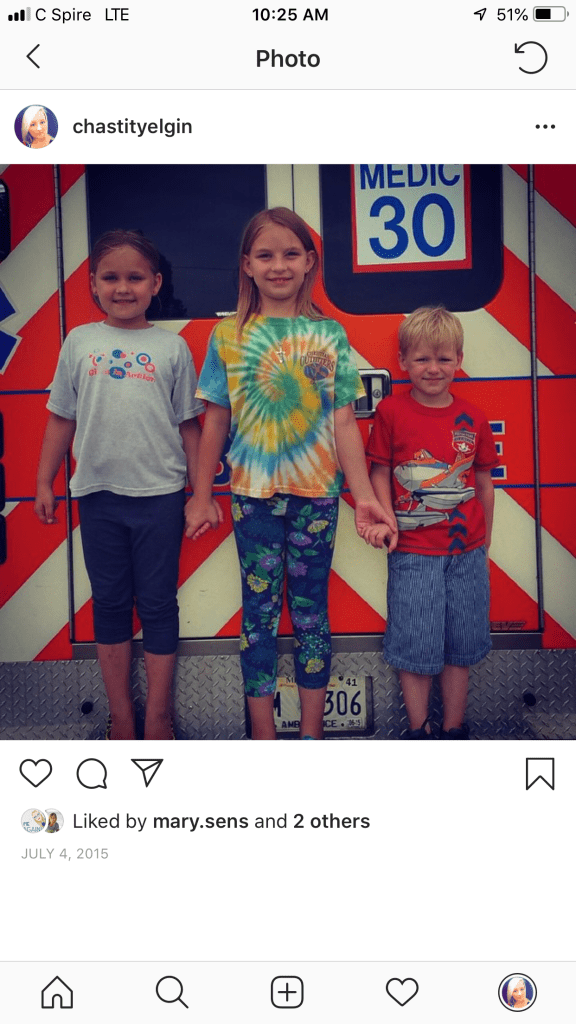
My oldest is about to graduate high school. My middle daughter will walk the stage next year, and my youngest—my son—is almost 15. They’ve grown up with the sound of scanner traffic in the background and me rushing out the door before the sun comes up. They’ve learned to expect late dinners, missed holidays, and rescheduled birthdays.
Sure, they take pride in what I do—there’s something special about being the kid whose mom drives an ambulance. But there were so many times when I pulled up to their school for lunch, a play, or an award ceremony… and the tones dropped before I could even get out of the truck. I’d cry silently on the way to a call, heartbroken that I missed another moment I couldn’t get back.
I’ve since made a promise: if I can’t find coverage, I’ll call out for their events. Because as much as I love my job, they’re more important. My kids only get one momma.. EMS gets the rest of me.
They’ve gotten different versions of me over the years. I can be overprotective. I’ve made them wear life vests in two feet of water. I slap on Band-Aids when they might have needed stitches. I overthink every cough, every fever, every bump on the head—because I’ve seen what happens when the worst-case scenario becomes someone’s reality. I know they get frustrated, but it all comes from love… and fear I want to be there for everyone. But I want to be there for them first.

How Communities Are Affected
People don’t always understand the shortage until it touches their lives. But I can say with confidence: some have lost loved ones because help didn’t arrive fast enough. That’s not fear-mongering. It’s just the truth. Every minute matters in an emergency, and when no ambulance is available—or the closest one is 30 miles away—that minute becomes a gamble with someone’s life.
I wish more people could see what we do up close—the good, the bad, and the beautiful. That’s why I love educating new EMTs, showing kids the truck, letting them flip the lights on, and answering questions about when to call 911. Those wide eyes might one day belong to a future paramedic. And maybe—just maybe—those small moments can help rebuild the broken pieces of this broken system. We’re not trying to be heroes. We’re just doing the best we can. But we can’t do it alone.
Solutions in Sight – Where Do We Go From Here?
The shortage of paramedics is real, and it’s affecting all of us. But it’s not all doom and gloom—there are steps we can take, both as professionals and as a community, to start moving in the right direction.
Public Awareness: Knowing When to Call 911
One of the biggest ways the public can help? Understanding when to call an ambulance—and when not to.
We’re not saying don’t call us—we’re saying know when it’s truly needed. Every day, EMS responds to calls that could be handled in a clinic, urgent care, or primary care office. A sore throat that’s been there for three days? A stubbed toe from the night before? These aren’t emergencies. But they still tie up ambulances that might be needed for someone having a stroke or a heart attack.
That’s where public education comes in. We need to do a better job of explaining what qualifies as a 911 emergency—and how to access care outside of emergency services. The more people understand how the system works, the better they can use it.
When an ambulance is delayed because it’s transporting a stable patient with a non-emergency complaint, someone in a true emergency might pay the price.
It’s not about blame. It’s about knowledge.
The Rise of Advanced EMTs: A Bridge in the Gap
With a nationwide shortage of paramedics, Advanced EMTs (AEMTs) are becoming a crucial part of the solution. AEMTs can do more than a basic EMT—they can start IVs, give some medications, and provide more advanced care in the field. They don’t require as much training as a paramedic, which means we can train and deploy them faster while still maintaining a high standard of care.
They are the middle ground we desperately need right now—a bridge between the gaps left by paramedic shortages. And just like the rest of us in this field, they’re not here for fame or fortune. They’re here because they care. You don’t go into EMS for money—you do it because you have a heart for helping people on their worst day.
Next Steps for the System
Here’s what we can do moving forward:
- Support EMS education by funding programs that encourage students to pursue this path.
- Incentivize staying in the field with better pay, mental health resources, and room for growth.
- Encourage career advancement from EMT to AEMT to Paramedic through streamlined training pipelines.
- Push for public campaigns about 911 usage, emergency preparedness, and when to seek alternate care.
- Partner with schools to introduce EMS careers early to students, sparking interest before they graduate.
And one more thing—we need to show appreciation for every role in EMS, not just paramedics. EMTs are often the first step in the chain of survival. They’re the first faces people see when they call for help. They assess, assist, and transport patients with professionalism and compassion, day in and day out.
And our EMS drivers? They’re the ones navigating traffic, dodging dangers, and getting us to scenes safely—often while we’re working in the back of a moving vehicle. Without them, none of this works. Every role matters. Every person counts. From the EMT fresh out of class to the seasoned paramedic on their final shift, and everyone in between—this system runs because of their dedication.
We didn’t get here overnight, and we won’t fix it overnight either. But step by step, call by call, conversation by conversation—we can make progress. Because the truth is, EMS isn’t just about lights and sirens. It’s about showing up, every single time, even when it hurts. Even when we’re tired. Even when the odds are stacked against us.
And with the right support, we will keep showing up.
The Final Call – A Message to the Nation
To the reader, if you’ve made it this far, thank you.
Thank you for taking the time to learn about what it really means to be in EMS. Not the TV version, not the dramatic movie scenes—the real, raw, unfiltered truth.
This blog isn’t just a collection of stories or complaints. It’s a lifeline. A plea. A call to action from the men and women who are out here giving it their all, day after day, shift after shift—with tired eyes, sore backs, and hearts that have carried more than they ever thought they could.
This is a system that’s stretched thin. It’s bleeding. And it needs help.

We Can’t Do This Alone
It takes more than medics to make this work. It takes:
- Policymakers willing to fight for better pay, benefits, and staffing.
- Communities willing to support their local EMS teams and learn how and when to use emergency services.
- Future generations willing to step up and carry the torch.
- Families willing to understand the sacrifices made behind the scenes.
- And it takes a country that sees us—not just as sirens in the distance, but as people with stories, families, and a mission.
To My Brothers and Sisters in EMS
This one’s for you.
To the EMT running back-to-back calls in an underfunded system.
To the AEMT filling in the gaps and going the extra mile.
To the EMS driver who dodges cars, potholes, and chaos to get us there safely.
To the Paramedic still wiping away tears from a call 10 years ago.
To the medic who clocked in today knowing they’ll miss a birthday, a ballgame, or bedtime—again.
You are seen. You are valued. You are essential. This profession is heavy, but it’s holy work. The kind of work that changes lives—sometimes in ways we’ll never fully understand.
A Message to America
So where do we go from here?
We start by listening. By showing gratitude. By sharing what we’ve learned. By voting for leaders who will prioritize healthcare infrastructure. By supporting training programs and breaking down barriers to entry. And by never taking for granted the ones who show up when it matters most.
The next time you see an ambulance pass, take a moment to think about who’s inside. Not just the patient—but the crew. The ones who left their own families to care for someone else’s. The ones running toward the unknown, because it’s what we do.
This is the final call of this blog—but not the end of the story.
Because the truth is, we’re still out there.
Still suiting up. Still saying the prayers. Still taking the calls.
And if we work together, maybe—just maybe—we can make sure there’s always someone to answer when the next call comes in.

“Send Me”
“Then I heard the voice of the Lord saying,
‘Whom shall I send?
And who will go for us?’
And I said,
‘Here am I. Send me!’”
— Isaiah 6:8 (NIV)
A Favorite of mine——
The Paramedic’s Prayer
Lord, grant me the wisdom so that I may treat those of Your children who lay at my feet.Let me
see only a patient and not a crime,
A person and not a circumstance.
Help me to stay strong, so I may carry those who can’t go on,
And to be gentle when life hangs in the balance.
Give me steady hands, a calm heart,
And courage beyond fear.
When the call comes in and the sirens wail,
Ride with me, Lord, through the chaos and the unknown.
And when my shift is over,
Allow me to return home safely to those I love.
But if, in Your will, I should give my life for another—
Then let me do it with honor,
Just as You gave Yours for me.
Amen.
-author unknown
So God Made a Paramedic
And on the eighth day, God looked down on His planned creation and said,
“I need someone to run toward danger when everyone else runs away.”
So God made a Paramedic.
God said, “I need someone strong enough to carry another’s weight—
yet gentle enough to hold the hand of a dying stranger.
I need someone to wake before dawn, work through the night,
miss holidays, birthdays, and ballgames,
and still be ready to answer the next call with compassion and grace.”
So God made a Paramedic.
“I need someone who can think clearly under pressure,
drive fast but safe, lift without breaking,
listen without judging,
and care without question.
Someone who will face trauma, tragedy, heartbreak, and horror—
then somehow go home and kiss their kids goodnight.”
So God made a Paramedic.
God said, “I need someone who won’t back down from the hard calls,
who will keep calm in the chaos,
cry in silence when the world’s asleep,
and still show up tomorrow to do it all again.”
So God made a Paramedic.
“I need someone with a soul tough enough for the streets,
but soft enough to comfort the broken.
Someone who will hold the line,
even when no one’s watching.
And who—when the final call comes—
will stand ready, still willing to serve.”
So God made a Paramedic.
- Author unknown
If you like my blog, be sure to share it 🙂 Thanks, Have a blessed day!
Chastity Elgin